
How Engineering Teams Build Scalable Telemedicine Platforms
A video call with a doctor may feel simple, but it relies on a much deeper technical foundation. That connection is only the tip of a vast iceberg. Modern telemedicine platforms are not apps. They are complex distributed systems. They must handle sensitive data, guarantee uptime, and serve a sudden rush of users without a stutter.
Building them requires engineering discipline from the first line of code. You can't just bolt scale on later. The architecture decides your fate.
Why Scalability Matters in Modern Telemedicine Platforms
A platform that works for a hundred patients will choke on a thousand. Scalability isn't a feature. It's the main event. These systems face unpredictable, spiky demand, such as Monday mornings or the release of a new health advisory. They juggle real-time video, persistent data streams, and integrations with hospital records. If performance dips during a consultation, trust evaporates.
The pressure points are brutally consistent:
- Rapid growth in remote consultations and users;
- Uneven load during peak hours;
- Dependence on video, real-time data, and multiple integrations;
- High availability requirements even under heavy traffic.
Engineers must design for these surges from day one. A crash during peak hours isn't a minor bug. It's a clinical and business failure that's incredibly hard to come back from.
Core Architecture Behind Scalable Telehealth Solutions
The wrong foundation will buckle. Early choices about structure lock in future limits. A monolithic application, where all code is one interconnected block, might get you to market faster. But when you need to scale just the video component, you're scaling everything, the whole costly, clunky mass. That's a recipe for waste and fragility.
Monolithic vs Modular Approaches in Telehealth
Modular, or microservices, architecture breaks the system into discrete, communicating parts. The video service, the messaging service, and the patient data service operate independently. This approach reflects the reality of modern scalable healthcare software.
The advantages become clear quickly:
- Separation of core services and user-facing features;
- Independent scaling of video, messaging, and data layers;
- Fault isolation across critical components;
- Easier long-term maintenance.
If the video service has a problem, the messaging and data services can, in theory, keep humming. That's resilience. It's also more complex to build and oversee, a classic trade-off. But for scale, it's often the only sane path.
Telemedicine App Development as a System-Level Process
The patient sees an app. Engineers see a constellation of services. Telemedicine app development is this system-level orchestration. It's the coordination of backend APIs, mobile clients, cloud infrastructure, and third-party integrations like EHRs. Teams at firms like Yalantis approach it this way, treating the frontend as one output of a much larger machine.
Success hinges on parallel work streams and shared foresight:
- Coordination between backend, mobile, and cloud teams;
- Early planning for load, latency, and security;
- Alignment with healthcare compliance requirements;
- Support for future feature expansion.
You model load patterns before writing UI code. You decide on data encryption standards before picking a database. It's a mindset that considers the legal, technical, and user experience domains as one tangled problem.
Remote Patient Monitoring and Data-Driven Care
Add connected devices, and the game changes again. Now the platform isn't just managing scheduled calls. It ingests a constant drip of biometrics, including heart rhythms, glucose levels, and sleep data. This turns a transactional system into a streaming data hub. Architecture must shift to handle this firehose of small, critical packets.
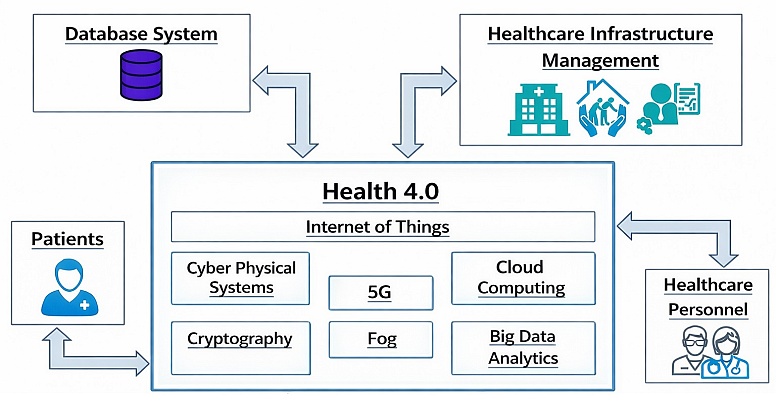
Handling Continuous Data Streams from Medical Devices
This data is noisy, personal, and time-sensitive. The system must validate it, spot outliers that might indicate an event, store it securely, and surface it for a clinician without stupid lag.
The technical checklist gets longer:
- Continuous ingestion of health metrics;
- Data validation and anomaly detection;
- Secure storage of sensitive medical data;
- Near real-time access for clinicians.
A batch job that runs every hour is useless here. The infrastructure needs a streaming data pipeline, maybe with Kafka or similar, to process this flow as it arrives. It's a different beast from request-response web traffic.
Security, Compliance, and Reliability at Scale
In healthcare, security is not a plugin. It's the fabric. Compliance rules like HIPAA aren't suggestions. They're hard constraints that shape database design, access logs, and even how you write error messages. Building for scale means these requirements must scale too, automatically, without becoming a manual checklist for ops teams.
The non-negotiables stack up:
- Protection of patient data across all layers;
- Access control for different user roles;
- Audit readiness and traceability;
- Resilience against system failures.
Every engineer must code with the auditor looking over their shoulder. A system that scales but can't prove who accessed a record at 2 AM is a failed system. Reliability here is about legal defensibility as much as uptime.
Infrastructure Choices for Growing Telehealth Platforms
The cloud is the obvious stage for this. But using the cloud isn't just about renting servers. In telehealth app development, adopting a cloud-native posture means relying on managed services, automating deployment, and designing for failure from the start. Your infrastructure code becomes as important as your application code.
Key decisions focus on elasticity and control:
- Cloud-native deployment models;
- Auto-scaling for fluctuating demand;
- Redundancy and failover strategies;
- Cost control at scale.
Auto-scaling groups spin up servers during a demand spike and spin them down afterwards. Load balancers distribute traffic. Database read-replicas handle queries. You pay for what you use, but you also have to architect to avoid runaway costs when something, inevitably, goes a bit sideways.
Key Engineering Challenges in Scaling Telemedicine Platforms

The work never really ends. Each victory reveals a new set of problems. You get the video stable, then realize your billing service can't keep up with the new user volume. The platform is a living thing, and growth stresses every joint.
The chronic challenges are predictable but tough:
- Balancing performance and cost;
- Maintaining quality during rapid growth;
- Integrating third-party healthcare systems;
- Supporting long-term platform evolution.
That last one is a killer. Technology stacks age. New regulations appear. You must build with enough abstraction that you can swap out a video provider or a database without rebuilding the universe. It's a marathon of constant, careful refactoring.
A scalable telemedicine platform isn't a product of one brilliant API or a trendy framework. It's the result of a thousand systemic engineering choices made with the next five years in mind. It's the boring stuff, like clean service boundaries, comprehensive logs, and automated recovery procedures, that lets the magic of a simple doctor's visit happen reliably for the hundredth or the hundred-thousandth time.
The real engineering happens far from the user's screen, in the messy, vital plumbing that makes it all seem effortless.














